2026 Guide: Maximizing Medicaid Waivers for Special Needs Services
Understanding and leveraging Medicaid waivers is crucial for US families seeking comprehensive special needs services in 2026, providing vital access to home and community-based care.
Navigating the complex landscape of special needs care can be daunting for US families. However, Medicaid waivers special needs services offer a critical lifeline, providing essential support that enables individuals with disabilities to thrive within their communities. This guide outlines practical steps for families to understand, access, and maximize these vital resources in 2026.
understanding Medicaid waivers: a 2026 perspective
Medicaid waivers, officially known as Home and Community-Based Services (HCBS) waivers, are state-specific programs designed to provide long-term care services in a person’s home or community rather than in institutions. In 2026, these waivers continue to be indispensable for families supporting individuals with special needs, offering a diverse array of services tailored to individual requirements. They play a crucial role in promoting independence and enhancing the quality of life for recipients, reflecting a shift towards person-centered care models.
The core purpose of these waivers is to prevent institutionalization and allow individuals to receive necessary care in less restrictive, more integrated settings. Each state operates its own set of waivers, meaning eligibility criteria, available services, and application processes can vary significantly. Staying informed about these state-specific nuances is paramount for families seeking to access these benefits effectively.
what are HCBS waivers exactly?
HCBS waivers are authorized under Section 1915(c) of the Social Security Act, allowing states to waive certain Medicaid requirements. This flexibility enables states to offer a broader range of services to specific target populations, such as individuals with intellectual or developmental disabilities, physical disabilities, or chronic medical conditions. These services often go beyond what traditional Medicaid covers, addressing critical needs that support daily living.
- Flexibility: States can tailor services to meet unique community needs.
- Community Integration: Promotes care in home and community settings.
- Cost-Effectiveness: Often more affordable than institutional care.
key changes and trends in 2026
As we move into 2026, several trends are shaping the landscape of Medicaid waivers. There’s an increased emphasis on person-centered planning, where individuals and their families have a greater say in designing their care plans. Technological advancements are also being integrated, with some waivers exploring telehealth, remote monitoring, and assistive technologies to enhance service delivery and accessibility. Understanding these evolving aspects can help families better advocate for their loved ones.
Another significant focus for 2026 is addressing workforce shortages in direct care. States are implementing strategies to recruit and retain qualified caregivers, which can impact the availability and quality of services. Families should stay updated on their state’s efforts in this area, as it directly affects the practical implementation of their waiver benefits.
In conclusion, understanding the fundamental nature of Medicaid waivers and keeping abreast of current trends in 2026 is the first vital step for families. These programs are dynamic, continuously adapting to meet the evolving needs of individuals with special needs and their caregivers.
eligibility criteria and application process for 2026
Navigating the eligibility requirements and application process for Medicaid waivers can feel like a labyrinth. However, a clear understanding of these steps is crucial for families in 2026. Eligibility typically involves both financial and functional criteria, which vary by state and by the specific waiver program. It’s not uncommon for families to find themselves overwhelmed by the paperwork and assessments, but persistence and meticulous record-keeping are key.
Generally, financial eligibility is tied to Medicaid’s income and asset limits, though some waivers employ special ‘medically needy’ income disregards for children and adults with disabilities, allowing higher income families to qualify. Functional eligibility, on the other hand, assesses an individual’s need for a level of care typically provided in an institution, such as a nursing home or intermediate care facility for individuals with intellectual disabilities. This assessment determines if the individual requires the intensive support that a waiver can provide.
financial eligibility considerations
For many families, financial eligibility is the first hurdle. While standard Medicaid income limits can be low, specific waiver programs often use an institutional deeming process, meaning only the applicant’s income and resources are considered, not the parents’ or spouse’s. This is particularly beneficial for children with disabilities. In 2026, families should investigate these specific rules within their state to determine if their loved one qualifies.
- Income Limits: Varies by state and waiver, often higher than general Medicaid.
- Asset Limits: Typically set at a certain threshold, though some assets may be exempt.
- Spend-Down Provisions: Some states allow individuals to ‘spend down’ excess income on medical expenses to qualify.
the functional assessment and level of care
The functional assessment is a critical component of the application. It involves a comprehensive evaluation by healthcare professionals to determine the individual’s need for assistance with activities of daily living (ADLs) and instrumental activities of daily living (IADLs), as well as cognitive and behavioral support needs. This assessment directly informs whether the individual meets the ‘level of care’ required for a specific waiver.
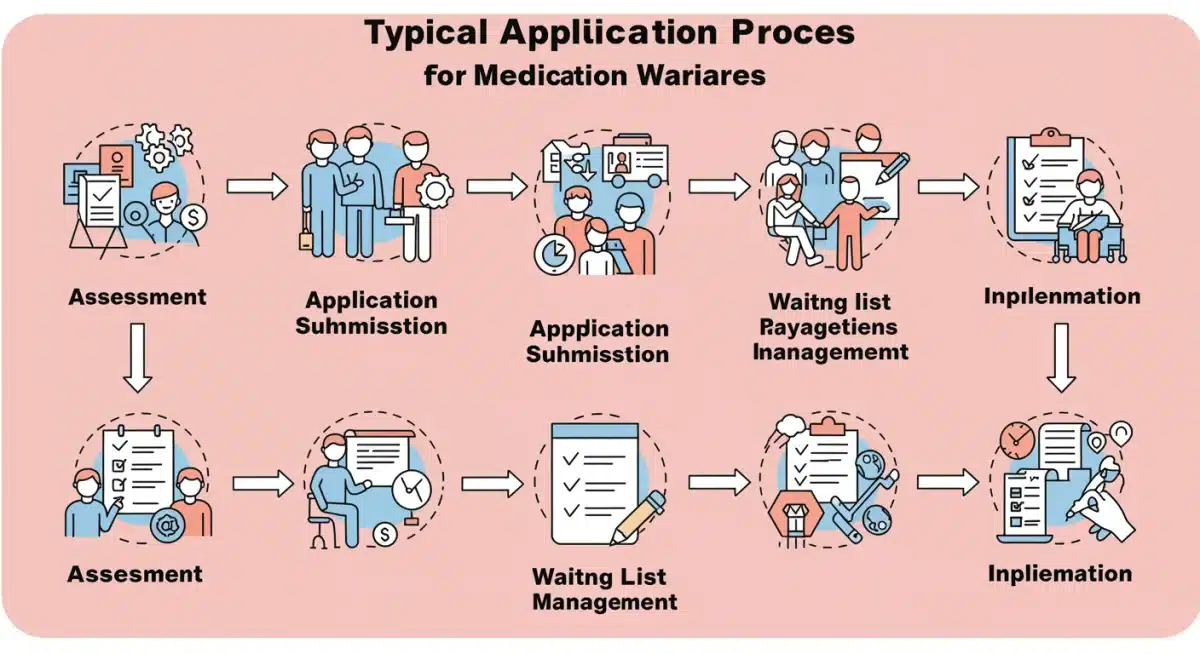
The application process itself often begins with contacting the state’s Medicaid agency or a local disability services office. Families will typically need to complete extensive forms, provide medical documentation, and participate in interviews. It’s advisable to gather all relevant medical records, diagnoses, and therapy reports beforehand to streamline the process.
Once deemed eligible, many waivers have waiting lists due to funding limitations. Understanding the length and management of these waiting lists in your state is crucial for planning. In summary, navigating eligibility and application requires diligence and a proactive approach, but the benefits of securing a waiver are immeasurable for families in need.
maximizing waiver benefits: services and supports in 2026
Once a family successfully secures a Medicaid waiver, the next critical step is understanding how to maximize the benefits and services available. In 2026, waivers offer a wide array of supports designed to cater to the diverse needs of individuals with disabilities, promoting their independence and inclusion within their communities. These services are not one-size-fits-all; they are intended to be personalized to each individual’s care plan, making careful planning essential.
The scope of services can include personal care assistance, skilled nursing, therapies (physical, occupational, speech), respite care for family caregivers, home modifications for accessibility, assistive technology, and even specialized medical equipment. Furthermore, many waivers provide support for employment services, community integration activities, and transportation, all aimed at fostering a holistic approach to care.
personal care and daily living assistance
A significant component of many waivers is personal care assistance, which helps individuals with ADLs such as bathing, dressing, eating, and mobility. In 2026, there’s an increasing focus on consumer-directed care models, where individuals and their families have greater control over choosing and managing their care providers. This empowers families to select caregivers who best fit their specific needs and preferences, fostering a more personalized and effective care environment.
- Caregiver Choice: Ability to select preferred personal care providers.
- Flexible Scheduling: Adapting care to individual routines.
- Training and Support: Resources for family caregivers to manage care.
therapy services and assistive technology
Therapeutic services, including physical, occupational, and speech therapy, are often covered, playing a vital role in maintaining and improving an individual’s functional abilities. With advancements in assistive technology, waivers in 2026 are increasingly covering devices and modifications that enhance communication, mobility, and independence. This can range from adaptive communication devices to smart home technologies that support daily living.
Respite care is another invaluable service, offering temporary relief for primary family caregivers. This allows caregivers to rest and recharge, preventing burnout and ensuring they can continue to provide high-quality care. Families should actively explore all available services within their specific waiver program and advocate for a comprehensive care plan that addresses every aspect of their loved one’s needs, from daily assistance to therapeutic interventions and technological support.
In essence, maximizing waiver benefits involves a thorough understanding of the services covered, proactive planning, and effective communication with care coordinators to ensure all eligible supports are utilized to their fullest potential.
state-specific programs and regional variations in 2026
One of the most critical aspects of navigating Medicaid waivers in 2026 is recognizing the profound state-specific and regional variations. The United States operates a decentralized system, meaning each state designs and administers its own set of HCBS waivers. This leads to a complex patchwork of programs, each with unique names, eligibility criteria, service offerings, and even application processes. What might be available and accessible in one state could be entirely different in a neighboring one.
Families must understand that there is no universal ‘Medicaid waiver’ program. Instead, they need to research the specific waivers available in their state of residence. For instance, a waiver for individuals with intellectual disabilities in California might be structured very differently from a similar program in Texas or New York. These differences extend to funding levels, the number of individuals served, and the length of waiting lists.
researching your state’s waiver programs
The first step for any family is to identify the official state agency responsible for Medicaid and disability services. This is typically the Department of Health, Human Services, or a dedicated Department of Developmental Disabilities. Their websites are usually the best resource for detailed information on available waivers, eligibility, and how to apply. Look for programs specifically targeting the type of disability or special need your family member has.
- Official State Websites: Primary source for accurate information.
- Disability Advocacy Groups: Offer support and guidance on local programs.
- Local Service Agencies: Can provide direct assistance with applications.
understanding regional differences within states
Even within a single state, there can be regional variations in how waivers are implemented and which services are most readily available. Urban areas might have different service provider networks and resources compared to rural areas. These regional disparities can affect the practicality of accessing certain services, such as specialized therapists or transportation options. Families should connect with local disability resources and support groups to gain insights into these localized nuances.
Furthermore, waiting lists are a persistent challenge in many states. Some waivers have immediate availability, while others have waiting lists that can span years. Families need to inquire about the current status of waiting lists for relevant waivers and understand any prioritization criteria. Early application, even if the need isn’t immediate, can be a strategic move to secure a place on a waiting list.
In conclusion, a thorough investigation into your specific state’s Medicaid waiver programs and an awareness of regional differences are non-negotiable steps to effectively navigate and utilize these vital services in 2026. Proactive research and engagement with local resources will empower families to make informed decisions.
advocacy and navigating challenges for families
For US families in 2026, successfully accessing and sustaining Medicaid waiver services often requires a strong commitment to advocacy. The system, while designed to provide support, can be complex, bureaucratic, and sometimes challenging to navigate. Families frequently encounter hurdles ranging from lengthy waiting lists to disputes over service plans, making effective advocacy an indispensable skill. It’s about being an informed and persistent voice for your loved one’s needs.
One of the primary challenges families face is the sheer volume of paperwork and the often-confusing terminology. Keeping meticulous records of all communications, applications, assessments, and service plans is crucial. This documentation serves as a vital reference point and evidence should any disputes or appeals arise. Understanding the appeals process is also fundamental; if a service is denied or reduced, families have the right to challenge the decision.
effective communication with care coordinators
Care coordinators or case managers are often the primary point of contact for families within the waiver system. Establishing clear, consistent, and respectful communication with them is paramount. They can provide invaluable guidance, help interpret policy, and facilitate access to services. Families should prepare for meetings by outlining questions and concerns, ensuring all critical topics are addressed.
- Document Everything: Keep records of all interactions and decisions.
- Ask Questions: Clarify any confusing terms or processes.
- Follow Up: Confirm actions and timelines in writing.
joining support groups and advocacy organizations
Families do not have to navigate this journey alone. Joining local and national support groups and disability advocacy organizations can provide a wealth of information, emotional support, and practical strategies. These groups often share experiences, tips for navigating specific state systems, and can connect families with legal aid or specialized advocates. In 2026, online forums and social media groups also offer accessible platforms for peer support and information exchange.
Advocacy also extends to participating in public hearings or surveys related to Medicaid programs. Sharing personal stories and experiences can influence policy decisions and highlight areas where improvements are needed. Legislators and policymakers often rely on constituent feedback to shape future legislation and funding allocations. Being an active participant in these processes ensures that the voices of individuals with special needs and their families are heard.
Ultimately, navigating the challenges of Medicaid waivers requires resilience, informed advocacy, and a willingness to seek support from various resources. By being proactive and persistent, families can significantly improve their loved one’s access to essential care and services.
future outlook: Medicaid waivers in a changing healthcare landscape 2026
As we look towards the future, specifically in 2026 and beyond, Medicaid waivers are poised to adapt within an ever-evolving healthcare landscape. The trends we observe today—such as the increasing integration of technology, a stronger emphasis on value-based care, and continued efforts to address health equity—will undoubtedly shape how these critical services are delivered and accessed. Families need to remain aware of these broader shifts to anticipate potential changes and continue advocating for robust support systems.
One significant area of focus is the push for greater efficiency and accountability in healthcare spending. This could lead to more refined outcome measures for waiver services, ensuring that programs are not only accessible but also demonstrably effective in improving the lives of recipients. The goal is to maximize the impact of every dollar spent, which could translate into more data-driven decision-making regarding service provision and program design. This might also mean increased scrutiny on care plans to ensure they are truly person-centered and achieving desired results.
technological integration and access
The acceleration of telehealth and remote monitoring during recent years has highlighted the potential for technology to expand access to care, especially in rural or underserved areas. In 2026, we can expect to see further integration of these technologies into waiver services. This could include remote therapy sessions, virtual care coordination meetings, and assistive technologies that enhance independence at home. For families, this means exploring how these tech-driven solutions can be incorporated into their loved one’s care plan to bridge gaps in traditional service delivery.
- Telehealth Expansion: Virtual consultations and therapy sessions.
- Remote Monitoring: Enhanced safety and support at home.
- Assistive Tech Funding: Increased coverage for innovative devices.
addressing workforce challenges and equity
The direct care workforce shortage remains a persistent challenge that will likely continue to influence waiver services. Initiatives to recruit, train, and retain qualified caregivers will be crucial. Families should stay informed about state and federal efforts to bolster this workforce, as it directly impacts the availability and quality of hands-on care. Furthermore, there’s a growing recognition of the need to address health disparities and ensure equitable access to waivers across all communities, regardless of socioeconomic status or geographic location.
Policy discussions in 2026 might also revolve around simplifying the application process, reducing administrative burdens for families, and streamlining inter-agency coordination. The aim is to make the system more user-friendly and less daunting, ensuring that families can focus more on care and less on bureaucracy. Staying engaged with advocacy groups and legislative updates will be vital for families to contribute to and benefit from these evolving changes.
In conclusion, the future of Medicaid waivers in 2026 is dynamic, marked by technological advancements, a focus on efficiency, and ongoing efforts to enhance equity and access. Families who remain informed and engaged will be best positioned to navigate these changes and continue to secure optimal care for their loved ones.
practical steps for US families in 2026
For US families supporting individuals with special needs, taking practical, actionable steps is essential to effectively navigate and maximize Medicaid waivers in 2026. This isn’t just about understanding the system; it’s about strategic planning and consistent execution to ensure your loved one receives the comprehensive care they deserve. The journey can be long, but with a structured approach, families can feel more empowered and achieve better outcomes.
The first practical step involves thorough research. Before initiating any applications, invest time in understanding the specific waiver programs available in your state. Visit your state’s Medicaid website, look for dedicated disability services portals, and identify the waivers that align with your family member’s diagnosis and needs. Pay close attention to eligibility criteria, covered services, and any current waiting list information.
organizing documentation and records
Once you’ve identified potential waivers, begin compiling all necessary documentation. This includes medical records, diagnoses, therapy reports, financial statements, and proof of residency. Create an organized system, whether it’s a physical binder or a digital folder, to keep everything easily accessible. This will save significant time and reduce stress during the application process, and provide a clear history if any appeals are needed.
- Medical Records: Keep all diagnoses, assessments, and treatment plans.
- Financial Documents: Gather income statements and asset information.
- Communication Log: Document all interactions with agencies and providers.
engaging with support networks and professionals
Do not hesitate to seek assistance from professionals and support networks. Connect with a disability advocate, a social worker, or an attorney specializing in special needs law if complex issues arise. These experts can offer invaluable guidance, help interpret regulations, and assist with appeals. Furthermore, joining local parent support groups or online communities can provide peer advice, share best practices, and offer emotional solidarity.
Proactive communication with care coordinators is also paramount. Regularly check in, ask clarifying questions, and ensure that your loved one’s care plan is being implemented as agreed upon. Be prepared to advocate for modifications or additional services if needs change. Remember, the goal is to create a dynamic care plan that evolves with the individual.
Finally, stay informed about policy changes at both state and federal levels. Legislation and funding can shift, impacting waiver availability and services. Subscribing to newsletters from disability organizations or government agencies can keep you updated. By combining thorough preparation, proactive engagement, and continuous advocacy, US families can effectively navigate Medicaid waivers and secure essential special needs services in 2026.
| Key Point | Brief Description |
|---|---|
| Understanding Waivers | Medicaid HCBS waivers offer home and community-based care, preventing institutionalization for individuals with special needs. |
| Eligibility & Application | Financial and functional criteria vary by state; meticulous documentation and assessment are crucial for application. |
| Maximizing Benefits | Utilize personal care, therapies, assistive technology, and respite care tailored to individual needs through personalized care plans. |
| Advocacy & Future | Proactive advocacy, staying informed about policy changes, and leveraging support networks are vital for long-term success. |
frequently asked questions about Medicaid waivers
In 2026, the primary types of Medicaid waivers typically include those for individuals with intellectual/developmental disabilities, physical disabilities, and specific medical conditions. Each state may have multiple waivers targeting different populations, offering a range of home and community-based services to prevent institutionalization and support independent living.
Financial eligibility for Medicaid waivers often differs from standard Medicaid through ‘institutional deeming.’ This means only the applicant’s income and assets are considered, not those of parents or spouses, allowing more individuals with disabilities to qualify even if their family’s income is above traditional Medicaid limits. Specific rules vary by state and waiver program.
A care coordinator, or case manager, is crucial for managing waiver services. They help individuals and families navigate the system, develop personalized care plans, connect with service providers, and ensure services are delivered effectively. They serve as a primary point of contact and advocate within the complex waiver framework.
Many Medicaid waivers in 2026 offer consumer-directed care models, allowing families to have significant input, and often direct control, over choosing their service providers. This empowers families to select caregivers and agencies that best meet their loved one’s specific needs and preferences, fostering greater personalization and satisfaction with care.
If a waiver application is denied or services are reduced, families should immediately inquire about the appeals process. They have the right to challenge these decisions. Gathering all relevant documentation, seeking advice from disability advocates or legal professionals, and clearly articulating their needs are crucial steps during an appeal to ensure fair consideration.
conclusion
Navigating the intricacies of Medicaid waivers special needs services in 2026 is undoubtedly a significant undertaking for US families. However, with a proactive approach, diligent research into state-specific programs, and persistent advocacy, these vital resources can unlock a world of support, enabling individuals with disabilities to live more independent and fulfilling lives within their communities. By staying informed about evolving policies, embracing available technologies, and leveraging robust support networks, families can effectively maximize these waivers, ensuring their loved ones receive the high-quality, person-centered care they deserve, now and in the future.





